Brief history of Keratoconus
The cornea is the clear window on the front of the eye. It provides the majority of the focussing power of the eye. Keratoconus (conical cornea) is a relatively common, bilateral condition affecting the cornea, occurring in more than 1 in 2000 people. It is characterised by corneal thinning and stretching which gradually progresses in both eyes. The result is a bulging forward of the cornea, resulting in an irregular cone shape. As a result, the eye develops irregular astigmatism and the vision may become severely blurred.
The condition typically starts in adolescence and early adulthood. Initial management is with glasses or rigid contact lenses. Replacement of the central cornea by corneal transplantation surgery becomes necessary in a minority of affected individuals when vision can no longer be improved with glasses or contact lenses.
What is Corneal Cross-Linking?
Corneal cross-linking is a new technique of collagen cross-linking using riboflavin (vitamin B2) and ultraviolet light (UVA). The goal of the surgery is to strengthen the collagen fibres within the cornea and halt or slow down progression of the thinning and “bulging” of the cornea in Keratoconus. It is also useful for patients with Pellucid Marginal Degeneration and keratectasia (both progressive conditions which have similarities to Keratoconus). In extensive experimental studies in animal eyes (including biomechanical stress and strain measurements) researchers have demonstrated a significant increase in corneal rigidity or stiffness after collagen cross-linking using this riboflavin/UVA treatment.
A pilot clinical study in humans evaluated the effect of the new cross-linking method in patients with Keratoconus and showed that, in all treated eyes, progression of the condition was halted. To date there are over 100 patients who have shown encouraging results after a 2-5 year follow up.
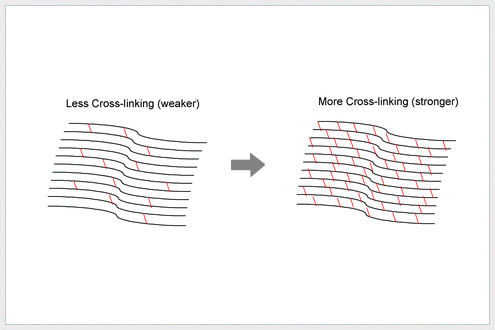
The theory behind CxL treatment is that in Keratoconus, the collagen fibrils of the cornea lose their ability to link to each other. CxL treatment aims to make more “links” between these fibrils, thus making the cornea stronger.
How is the treatment done?
The one-off treatment is performed under local anaesthesia with eye drops. It involves removing the top layer of tissue (epithelium) from the surface of the cornea, and then applying Riboflavin eye drops every 2 minutes, for 30 minutes in a measured dose. The depth of absorption is checked after 30 minutes to make sure the Riboflavin has penetrated to the required depth of tissue. The eye is then exposed to UVA light for 30 minutes (Riboflavin drops are continued during this time). After the treatment, a bandage contact lens is worn on the eye, and antibiotic ointment is applied until the surface of the eye has healed. The bandage contact lens can stay in place from 3-5 days depending on the rate of healing of the eye.
Immediately after surgery, the vision in the treated eye is blurry. This will improve over time as the eye heals. It may take some weeks for vision to be stable after this procedure.
Who can benefit from this treatment?
It is important to understand that collagen cross-linking treatment is not a cure for Keratoconus. Rather, it aims to slow or even halt the progression of the condition. After the treatment, it is expected that it will continue to be necessary to wear spectacles or contact lenses (although a change in the prescription may be required). However, the treatment will help prevent further deterioration in the condition and the need for corneal transplantation. Your own contact lenses (i.e the ones you would have been wearing before having CXL) can be worn after 4 weeks following the procedure. New contact lenses should not be fitted until after 3-6 months post-operatively.
A person with severe Keratoconus is unlikely to gain any benefit from this treatment. In this situation, other alternatives for treatment may need to be considered.